We get to know our periods very well through the course of our life. We can recognize the cramps and what they mean for the days ahead, we can gauge whether it’s going to be a heavy or light day, and we have a tell-tale list of signals and symptoms for the days leading up to the flow.
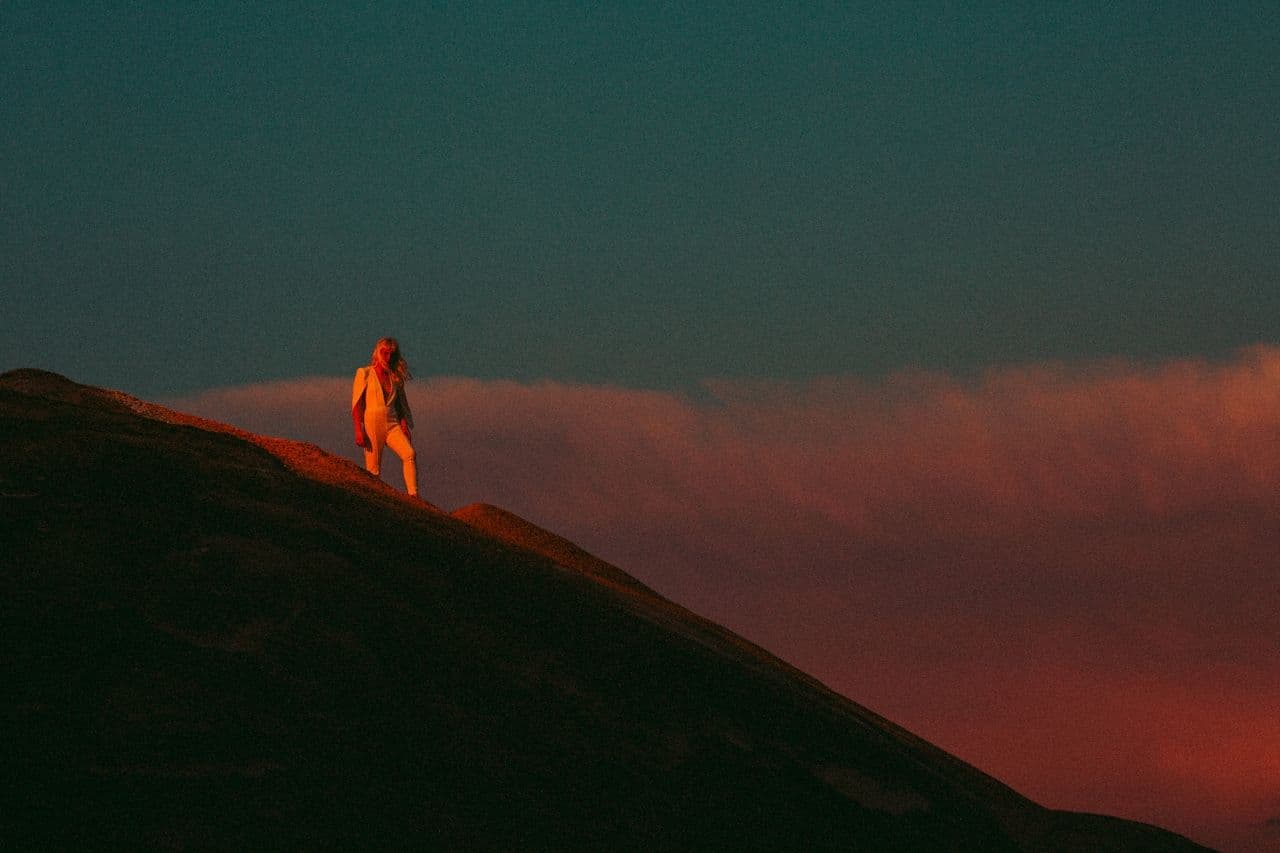
Cancer, as it does with most things, can scramble all this predictability. Many cancer treatments and associated drugs can affect your menstrual pattern, sometimes stopping your period altogether. Changes to your period can feel intense, almost feeling like cancer is taking away part of who you are.
“Losing your period can be symbolic and emotional,” says Dr. Kathryne Sanserino, a gynecologist at Stanford Medicine who works with cancer patients. “That’s normal and that’s a real feeling.”
Period changes can feel tumultuous, and experts say it’s normal for menstruation to be different and irregular during treatment. It can be a tricky adjustment to start going with your new flow, so we talked to gynecologists about what you can expect with menstruation during your cancer treatment and how you can manage the side effects.
Why Do Treatments Change Your Period?
In their quest to target rapidly growing cancer cells, some treatments like chemo and radiation–depending on the type, dosage, and anatomical location–may damage other cells, including those in the ovaries, the organs responsible for your reproductive function and periods.
There are also some estrogen-responsive cancers (like certain breast, ovarian, and endometrial cancers) that require hormone treatment (also known as endocrine treatment). These drugs suppress the production of estrogen, which also puts your reproductive system on pause.
Sometimes ovary-suppressing drugs are used to intentionally pause your period as a potential fertility preservation tactic or in order to prevent additional blood loss if your blood cell counts are low.
All of these forms of treatment can result in changes to your period; less is known about drugs like immunotherapies and targeted therapies. It is always best to ask your doctor about what changes to your period and fertility you should expect with your specific treatment plan.
What Period Changes Can You Expect?
Changes in your flow depend on several factors, including your typical menstrual patterns, age, and the type and dose of treatment you are receiving. Oftentimes, women stop having their period altogether, but some women experience a heavier flow, Penn Medicine gynecologist Dr. Suneeta Senapati says. “Both of those can, I think, be very alarming to patients who have a cyclicity or have a pattern that is normal for them that is all of a sudden disrupted.”
Your periods may stop as soon as you start treatment, or it may take some time before you notice any changes. This depends on where you are in your menstrual cycle when you start treatment, what the dosage of the treatment drugs are, and how strongly each specific drug affects your ovaries.
Some forms of chemo, as an example, are known to cause changes to menstrual cycles very quickly. In these cases, you may “stop menstruating pretty quickly, like within a couple of weeks to months,” says Dr. Senapati.
Your period may not feel or behave the same as it usually does. For example, you may experience spotting or irregularity, and that is also O.K. “It’s normal for it to be irregular, normal for you to just really not know what's going on,” Dr. Sanserino says. If you have specific questions about your menstruation patterns, talk to your oncologist about referring you to a gynecologist during your care.
Can I Get Pregnant Even If My Period Stops?
“It’s better to err on the side of caution and use contraception,” Dr. Sanserino says. Even though some cancer treatments pause menstruation, it can be irregular and you can still get pregnant. It’s crucially important to use contraception while undergoing treatment as many cancer treatments are incompatible with pregnancy. Also, if you’re doing a treatment like chemotherapy, you’ll want to use extra protection (like a condom) because the exchange of fluids can be harmful to your partner.
Do I Need to Change What Period Products I Use?
If you are undergoing treatment that makes you immunocompromised, oncologists may recommend staying away from products like menstrual cups or tampons. Dr. Sanserino says there isn’t much evidence supporting this, but rather that it comes from a general fear of introducing anything foreign into your body.
She suggests sticking with general precautions, “If while using the menstrual cup you notice that the vaginal tissue is very delicate and insertion is uncomfortable and perhaps causes an abrasion, discontinue use. We do not want any open wounds while immunocompromised!”
The same goes for tampons, which typically have an easier insertion and removal. As always, properly cleaning reusable products and practicing good hand hygiene when changing and reapplying them is also important. Dr. Sanserino also recommends using products free of scents or dyes that can be irritating to the vagina (she also recommends this for non-cancer patients).
Regardless of your preferences, open communication with your oncology team is important, Dr. Sanserino says. “It's always important to be open with your treatment team about what you are doing and consider their recommendations.”
Are There Other Side Effects?
In addition to disrupted flow, because these treatments are affecting ovarian function, you may experience menopausal-like side effects. This is especially common in women receiving hormonal or endocrine therapy for breast cancer, as those treatments are telling your body to stop producing estrogen, but they can occur from any treatments that affect the ovaries.
Side effects can include hot flashes, joint pain, brain fog, night sweats, and low sex drive, among others. Oftentimes these symptoms only last during treatment, but sometimes they can return or persist depending on your age and the treatment. Our guide to treatment-induced menopause here talks about these symptoms and some ways to alleviate them.
Will My Period Come Back?
Many people experience resumption of periods and end of menopausal symptoms following treatment, especially if they were younger upon starting cancer treatment.
“The hit to the ovary can cause a temporary cessation of periods or it can be permanent, so many people will stop menstruating just during their treatment and then months or years after treatment will resume menstruating. That's seen more often in patients who are under 40,” Dr. Sanserino says.
If you notice your period isn’t coming back, touch base with your gynecologist to check in on your reproductive health. You may also start noticing menopausal symptoms again, which can come as a shock. Talk to your doctor about whether treatment-induced menopause, menopause that occurs more suddenly and earlier than natural menopause, may be something you are experiencing.
What Does This Mean for My Fertility?
Experts say that resumption of periods alone does not necessarily indicate fertility. This can be frustrating, as you may be seeking answers about your fertility status after completing treatment. (More at Jadey’s Fertility Guide here.)
“It’s really hard to predict and there’s not one test that we can do to…say what’s your fertility status and what is going on with you,” Dr. Sanserino says.
Because some of these treatments are damaging to the ovaries, they may cause lasting damage or put you into early treatment-induced menopause. In some instances, it may mean complete loss of fertility after treatment. Experts recommend keeping in touch with gynecologic and fertility specialists to see what options are available to you, and to alleviate any menopausal symptoms.
“It is okay to reach back out to a fertility specialist, even if you saw them once before cancer treatment. See them after, just to have conversations about what to expect and to put together a care plan to navigate what may be coming ahead,” Dr. Senapati says.
Changes to your period can feel like a monumental shift in how you think about your body. It’s so normal to feel all sorts of ways about it. We’re here for all your gnarly, big feelings about your changing body, even as it may be hard to go with the flow.