Leading up to my surgery for ovarian cancer, I was terrified. But in my experience going through cancer treatment, I found that knowing what to expect tended to help calm my fears.
If you’re getting ready for gynecologic cancer surgery, this guide will give you the information you need. It combines need-to-know expertise from a gynecologic oncologist, as well as advice from several women (including me), who’ve gone through gynecologic surgery firsthand, so you know what to expect — and how to prepare.
The Most Common Gynecologic Cancer Surgeries
Gynecologic oncologist Dana Chase, MD, Professor of Clinical Obstetrics and Gynecology in the Division of Gynecologic Oncology at UCLA’s David Geffen School of Medicine, breaks down what to expect from the most common gynecologic cancer surgeries for the three most common gynecologic cancer types: endometrial, ovarian, and cervical.
Endometrial Cancer Surgery
Procedure: About 80% of people with endometrial cancer are diagnosed in stage 1 or 2, when the cancer is confined to the uterus and possibly a little outside of it into the nearby pelvic region. For early-stage endometrial cancer, the surgery is most likely going to be a minimally invasive procedure, says Dr. Chase. Rather than making a large incision, the surgeon will only need to make three to five very small incisions, each about the width of a fingertip, around the abdomen.
Endometrial cancer surgery typically involves a hysterectomy (removal of the uterus and cervix) and likely also a bilateral salpingo-oopherectomy (removal of both ovaries and fallopian tubes). In some instances when the cancer is only in the uterus and is not an aggressive type, the ovaries might not need to be removed, notes Dr. Chase.
When endometrial cancer is advanced and has spread beyond the uterus and into the ovaries, fallopian tubes, and/or more distant areas, open surgery (where a large vertical abdominal incision is made), is usually required, versus the minimally invasive procedures that can be used in the earlier stages. Open surgery for advanced endometrial cancer—and the recovery—is similar to the most common surgery for ovarian cancer. (See the Ovarian Cancer Surgery section below for more information.)
Hospital Stay: Minimally invasive surgery for endometrial cancer is usually an outpatient procedure, says Dr. Chase — meaning that if there aren’t any complications, you can go home the same day. If the surgery goes smoothly, it takes about two to three hours, and then you’re moved to the recovery room, where you’re monitored for another hour or two before being released.
Pain Management: This is going to vary because everyone has a different tolerance for pain, says Dr. Chase. “But because the incisions are so small [in minimally invasive surgery], usually the majority of patients have minimal pain; many times they’ll only need ibuprofen or Tylenol to manage it,” she says. The abdomen is inflated with air during minimally invasive surgery, so afterward you may feel gassy and bloated until that air dissipates, which usually takes one to two weeks, Dr. Chase adds.
Ovarian Cancer Surgery
Procedure: Ovarian cancer is the inverse of endometrial cancer, in that about 80% of people are diagnosed in stage 3 or 4, where the cancer has spread beyond the ovaries, fallopian tubes, uterus, pelvis, and it's moved further into the abdomen and beyond, says Dr. Chase, with only 20% diagnosed in the early stages. Because ovarian cancer is typically diagnosed when it’s already quite advanced, open surgery, rather than a minimally invasive one, is usually required.
In open surgery for ovarian cancer, a large vertical incision is made from above the belly button down to the pubic bone. Surgery for advanced ovarian cancer almost always includes removing the uterus and cervix, as well as both ovaries and fallopian tubes, says Dr. Chase.
Additionally, ovarian cancer surgery typically involves removing any visible tumors, which is called tumor debulking. Depending on how far the cancer has spread, tumors might need to be removed from the bowel, liver, spleen, and more, explains Dr. Chase. In some instances, when a large portion of the intestine needs to be removed due to cancer, you may need an ostomy, where stool is diverted to empty through a hole in your abdomen into an attached plastic pouch, called an ostomy bag. This is rare, she notes, but something that you should be aware of and talk about with your doctor prior to surgery to find out if it might apply to your circumstances.
To close the abdominal incision after open surgery, doctors will either use stitches in combination with surgical tape or glue, or surgical staples. If you have surgical staples, you’ll need to go back to your doctor’s office to have them removed about 10 days after surgery — ask your doctor about your specific timing. Again, the pain from this part of the process will depend on each individual’s tolerance. I had surgical staples in my incision and what I can say is: having them removed wasn’t as painful as I feared it would be. If you have a low pain tolerance or are very anxious about this, Dr. Chase says you can ask your doctor to use numbing gel on the area first.
For early-stage ovarian cancer, where the cancer is contained to the ovaries and nearby pelvic region, minimally invasive surgery is usually performed. That surgery—and recovery—is very similar to the minimally invasive procedure that's done for early-stage endometrial cancer. (See Endometrial Cancer Surgery section above for more information.)
Hospital Stay: Open surgery for advanced ovarian cancer usually takes from two to eight hours, depending on how extensive the surgery needs to be, Dr. Chase says. While minimally invasive surgery is typically an outpatient procedure, open surgery results in a longer recovery and requires an inpatient stay, usually for two to five days afterward.
Pain Management: Open surgery is also going to require more extensive pain management; ibuprofen and Tylenol alone typically won’t cut it and narcotics will usually be prescribed by your doctor. Dr. Chase also points out that sometimes an abdominal nerve block, a targeted injection to block pain, may be used during surgery to minimize post-operative pain and limit the need for narcotics. She recommends asking your anesthesiologist about nerve blocks at your pre-surgical appointment to learn more and see if they’re an option for you.
Cervical Cancer Surgery
Procedure: Cervical cancer is different from endometrial and ovarian cancers in that surgery is only performed on women with stage 1 cervical cancer. Even with stage 1, if the tumor is still confined to the cervix but it’s very large, surgery may no longer be an option. For cervical cancer that’s stage 2 and beyond, or a bulky stage 1, the recommended treatment is chemotherapy with radiation, sometimes with and sometimes without immunotherapy, explains Dr. Chase.
Studies have shown that open surgery results in better outcomes than minimally invasive surgery for those with early-stage cervical cancer who are candidates for surgery, so that’s typically what’s done, Dr. Chase says. This usually involves removing the cervix, uterus, and fallopian tubes. For women who are premenopausal, she says, the ovaries often don’t need to be removed. The incision is either made vertically down the midline of the abdomen, similar to the incision for open ovarian cancer surgery, or horizontally along the lower abdomen around the top edge of the pubic-hair line, which is called a Pfannenstiel incision, or informally referred to as a “bikini cut” incision.
Hospital Stay: Surgery typically takes between two to five hours and the hospital stay is normally about two to five days, says Dr. Chase.
Pain Management: Similar to open surgery for ovarian cancer, pain management after cervical cancer surgery usually involves the use of narcotics.
This is a general overview of the most common gynecologic surgeries for informational purposes only, and is not intended as medical advice. Each individual’s surgery is going to vary based on numerous factors including the extent and location of the cancer; talk to your doctor before your procedure to ensure you understand everything that your specific procedure will entail.
Gynecologic Cancer Surgery Recovery Tips
Recovering from gynecologic cancer surgery can bring a lot of challenges, from difficulties with daily tasks to something as seemingly simple as getting in and out of bed. We’ve compiled our favorite tips to help you navigate some of the most common post-op obstacles and make your recovery as smooth as possible.
Enlist help at home.
After both minimally invasive and open gynecologic cancer surgery, you should not lift, push, or pull anything over ten pounds for six weeks to three months, depending on your surgeon’s instructions, says Dr. Chase. Getting up from a squat to a standing position is actually equivalent to lifting about fourteen pounds, so these restrictions apply to more of your daily movements than you may think, she notes.
Additionally, you don’t realize how much you need your abdominal muscles for daily functioning until they’re severely impaired after abdominal surgery. For the first several days at home after my open ovarian cancer surgery, I practically couldn’t do anything for myself, from getting in and out of bed, to dressing and undressing, to tying my shoes. I lived alone at the time and my sister stayed with me for a week to help me with, well, everything.
If, like me, you don't have a live-in caregiver, see if a friend or family member can stay with you for at least a few days, recommends Dr. Chase. If there is no one who can stay with you, ask your care team or the hospital social worker about the possibility of going to an inpatient rehabilitation facility after your surgery, where you’ll be able to recover with around-the-clock assistance.
Shower with care.
Avoid taking a bath—or going swimming, sitting in a hot tub, or submerging your body in water in any way—for at least four to six weeks after both minimally invasive and open gynecologic cancer surgery, says Dr. Chase. It’s usually fine to shower fairly soon afterward, but between limited range of motion, fatigue, and fears about irritating incisions, showering after surgery can be daunting.
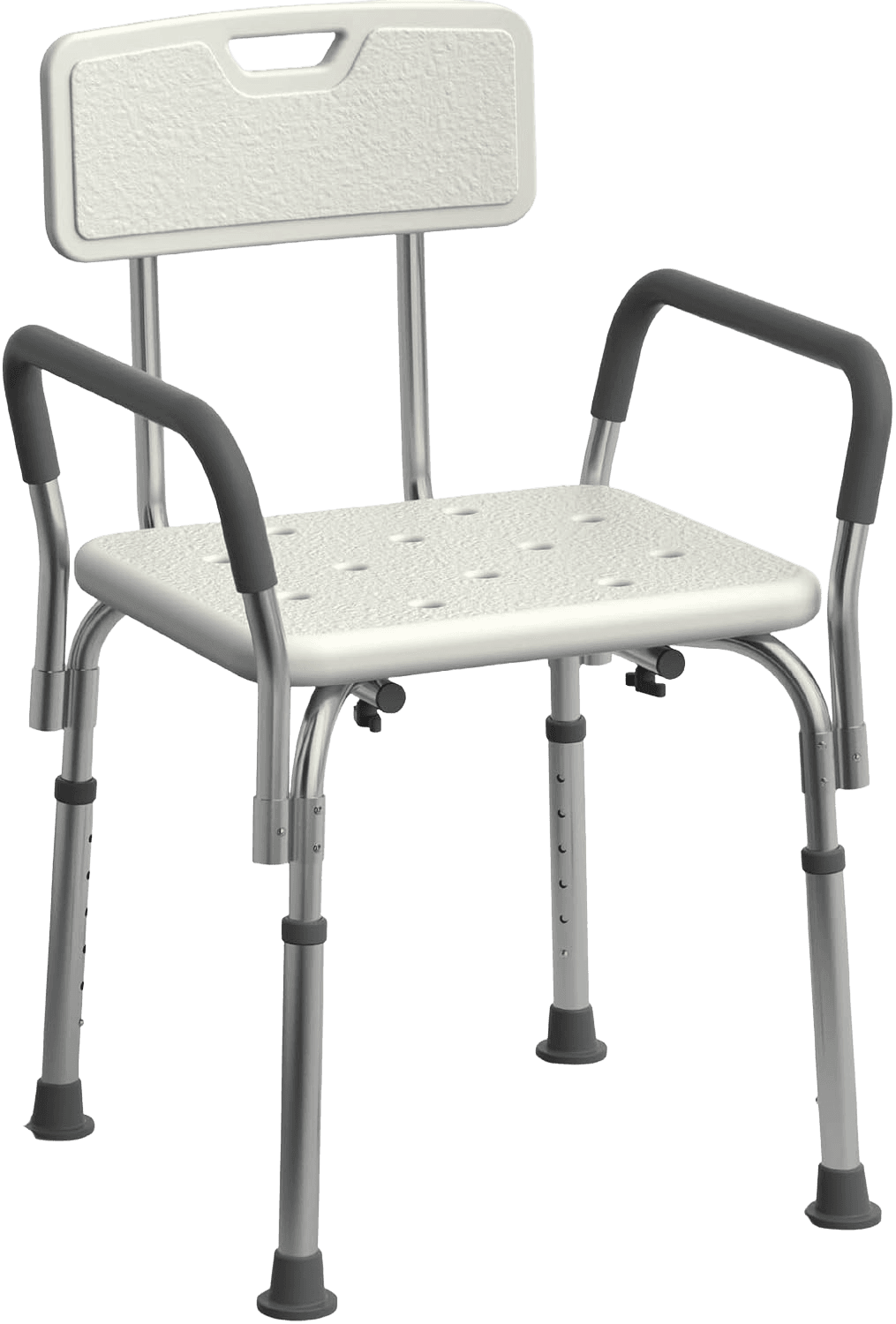
“Bathing was terrifying the first few days but having a shower chair was a huge help,” says Danille Glick, 42, a psychotherapist who had three surgeries related to cervical cancer. She also bought a removable shower head that had different speeds and pressures. “That way, I was able to clean myself carefully and in sections rather than all at once,” she says.
A removable shower head shouldn’t require professional installation, but you’ll definitely want to purchase and install it before surgery. Depending on how you’re feeling, and how handy you are, you may want to enlist help from a handyman or someone who’s good with DIY projects.
A note about incision care:
“Don't scrub your incision with soap, but if you use soap on the rest of your body, it’s okay for it to run over the incision area [while you’re showering],” says Dr. Chase. If there’s surgical tape or glue over your incision, that will protect the area even if water gets on it. However, if your doctor used surgical staples, they may want you to cover your incision with plastic, taped in place, when you shower, she adds.
“Make sure you understand your surgeon’s specific instructions for incision care,” Dr. Chase says.
When you dry off after showering, don’t rub a towel over your incisions, Danielle cautions. Be sure to very gently pat yourself dry instead.
Make your bathroom recovery-friendly.
In addition to a shower chair, an elevated toilet seat with arm rests can also be helpful for getting on and off the toilet without using abdominal strength, says Anna*, 44, a nurse who underwent surgery for ovarian cancer herself. After her own surgery, she used both. “Some insurances will cover the cost of these items,” she says. “If insurance doesn’t cover them, they can sometimes be obtained or borrowed from local cancer support organizations, or your hospital may have resources to help you get these items at no charge.”
You can also simply purchase items like a shower chair and elevated toilet seat and pay out of pocket. Just note that if you go this route you’ll have to assemble them yourself. When you obtain them through insurance they’ll be provided by what’s called a Durable Medical Equipment (DME) company, and you can request that the DME company deliver and assemble any products they provide.
Create a cozy sleep setup.
“Sleeping and getting in and out of bed was difficult after surgery,” says Nefa-Tari Moore, 45, Director of Black Women’s Outreach at SHARE Cancer Support and a former nurse who went through treatment for both endometrial and ovarian cancers. “I slept on my side hugging a big pillow, and also put one behind me to support my back,” she says.
Danielle had a similar setup, with the addition of a “reading pillow” with arm rests to use when sitting upright, as well as a special hysterectomy pillow to hug when coughing or sneezing in order to help protect abdominal incisions and minimize pain.
Both women recommend putting everything you may need — like your phone, TV remote control, any books you’re reading, a bottle of water, and medications — within reach on a nearby nightstand to keep you occupied and limit how often you have to get in and out of bed.
Stock up on loose, comfortable clothing — and super-soft underwear.
You do not want anything irritating your abdominal incision(s) after gynecologic cancer surgery.
“I wish someone had suggested either using a large gauze pad or a period pad in boy shorts or high-waisted underwear to prevent the underwear from rubbing along the incision,” Anna says. “Or even suggested that I go commando for the first few days to prevent major irritation.
“For the first six weeks post-op, I found high-waisted underwear or boxers to be the most comfortable, and after that I continued to wear high-waisted underwear for quite a long time,” she says.
Personally, I am a fan of disposable underwear they give you at the hospital. Before being released, I asked for extra pairs to take home with me. Not all hospitals are able to provide extra supplies, but it doesn’t hurt to ask. If the nurse won’t give you extra items like these to take home, Anna suggests asking to speak to the charge nurse, nurse manager, or social worker with your request. Explain that you need these supplies so you don’t have to go out to purchase them during the most difficult initial days of your recovery, especially if you live alone, she says.
For clothing, Anna recommends wearing soft, comfortable pants without any zippers or buttons that are loose-fitting enough that the waistband doesn’t dig into your abdomen. Button-down and zip-up shirts are easier to get on and off than anything you have to pull on over your head, she adds.
You may want to consider sizing up, especially for pants and underwear, to ensure that they’re loose enough.
Make meal prep easy…
Another thing that’s helpful to outsource while you’re recovering from surgery is cooking and grocery shopping — especially during the period when you need to avoid reaching and lifting.
Some people cook and freeze a bunch of meals in advance, says Dr. Chase. You could also ask people to drop off prepared meals and/or groceries, Anna suggests. “And if a friend or family member wants to set up a MealTrain for you,” she adds, “let them!”
When I was recovering from surgery, I had my groceries delivered; services like Amazon Fresh, Instacart, FreshDirect, and more make this easy. Because I lived on a higher floor of an apartment building, I wrote a note in my orders that I wanted the groceries brought directly to my apartment door rather than having to meet the delivery person in the lobby so I wouldn’t have to lift the heavy bags at all.
Beyond ordering takeout from your favorite restaurants, Anna points out that there are also some organizations that prepare and deliver free, medically tailored meals for people with serious illnesses like cancer — for example, God’s Love We Deliver in New York City and Ceres Community Project in Northern California. Ask the hospital social worker if there’s anything like this in your area.
… and outsource chores.
“Deep cleaning before surgery was a must for me, as well as making sure bigger loads of laundry were done,” Danielle says. “This is another area where it’s okay to ask for help — let someone else do the laundry or clean if they offer!”
“If you have a significant other, discuss with them what chores were usually yours that you are not going to be able to do for a bit… so they can pick up the slack while you recover,” Anna advises. There are even organizations that will clean your home for free while you are in cancer treatment, she notes.
When I had ovarian cancer I used Cleaning for a Reason, a national nonprofit that provides two free home cleanings for people who are going through cancer treatment. It can take a while to get placed with a cleaning service through them though, so apply as soon as possible. Just note that it can be a little tricky to try to coordinate the timing of your home-cleaning with your surgery and recovery and you may need to have a backup plan.
Finally: be very gentle with yourself.
In general, take it easy and try to offload as much as possible while you’re recovering.
“Everybody is different and will respond to surgery differently with what they are able to do post-op,” Anna says. “You have to listen to your body.”
The women we talked to who underwent gynecologic cancer surgery (including me) agree: be gentle with yourself, and ask for all the help and support you need. Especially while you’re recovering, it’s important to prioritize your own comfort, care, and well-being, whether that’s wearing the softest, most comfortable underwear; having friends drop off meals and help with household chores; or creating a cozy pillow sanctuary in your bed. Now is the time to focus on your own healing.
*First name only, at the subject’s request.